We spent 8 hours in the ER until they decided to admit Rebekah to the Peds Floor at Greenville Memorial Children's Hospital. They started Zofran to stop her vomiting in the hopes we calm her stomach enough to restart at least Pedialyte. But after running standard blood and urine cultures, it was determined that Rebekah had a pretty significant UTI. We still didn't know the strain, so they put her on IV Rocephin, and we figured in a day or two she would be back to normal. But it didn't go that way...
Because of the concern of the UTI extending to her kidneys, we did an abdominal ultrasound on 5/31. It showed no major issues of Rebekah's kidneys or liver. By Wed morning, Rebekah's tummy was becoming visibly distended. Rebekah continued vomiting despite the zofran, and was starting to vomit some bile here and there. All of this was a mystery since her blood work did not show anything significant (outside the UTI), and her white blood count numbers were actually going down.
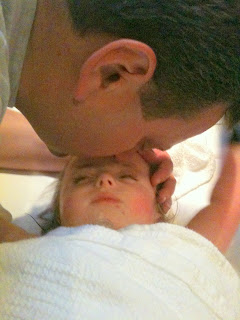 |
| Michael kissing Rebekah during the Upper GI Study |
An abdominal x-ray was ordered which showed a blockage in the smaller intestine. Because the doctors weren't sure if it was a complete blockage, they ordered an Upper GI Study to look at how things were digesting. To complicate matters, Rebekah had been on IV fluids since Monday evening, on IV Zofran for vomiting, and continued to vomit at least once every 3-4 hours. Her stomach was becoming more and more distended and the amount of bile backing up into the stomach was becoming significant.
 |
| Rebekah's distended tummy on Wed 6/1 |
For a period of about 12 hours, we attempted to administer multiple doses of barium to Rebekah for the upper GI x-ray series showing the progression of the barium through her tract. She kept vomiting the barium along with larger and larger amounts of bile. What little passed beyond the stomach was going no where. She was becoming more agitated and unconsolable. She absolutely did not want to be touched.
 |
| Rebekah's tummy on 6/2. The g-tube button was being pushed by so much pressure that it was sticking out was past the stomach. |
I said, "I am sure you don't need to be told this, but if Rebekah codes during surgery, or there are any major issues, you are to do every thing the can for her."
Well, his response pleasantly surprised me. "When we cross the door into the OR, we do absolutley everything we can for our patient. Even if they had a DNR, it would stop at the door and be ignored."
(Rebekah does NOT have a DNR (Do Not Resuscitate order), but his point was in the event of an emergency, they treat everyone equally. How refreshing!.
 |
| Dropping Rebekah off at the OR. Michael had to be at home for Isaiah's Kindergarten graduation. It's tough having to 'choose' between your children. :-( |
 |
| Rebekah's tummy when we picked her up post-op. Looks so much better! It will continue to shrink as she recovers from major abdominal surgery. |
 |
| Sweet Rebekah looking much better after surgery. Her face is relaxed and her lips actually have color. |
I want to end Part I of this story by sharing the story of Rebekah and her brother, Elijah. Rebekah has been miserable for this past week. She hasn't smiled at Mommy, Daddy, or even her Nurse Becky. She has been very grumpy for the nurses. But when her big brother showed up Wed night, she cracked a grin, touched his face, and even held his hand.
While that is a 'nice' story, I am telling it because there is a false assumption that trisomy kids are vegetables that are a burden to take care of and who will never know you. This is so far from the truth! Every trisomy 13 & 18 child I've met has a happy demeanor, a loving soul, and most definitely a recognition of their family. They are a special blessing, and sent to teach us about courage, hope, and unconditional love. I thank God so much for entrusting Rebekah to our family. It is where she belongs...


