Friday 6/3 - It is the day after surgery and Rebekah continues her pattern of sleeping. Even though I haven't seen her awake for more than a few minutes in 5 days, I still am not too worried. Her blood pressure had come down and she looks more comfortable and peaceful than she has in a long time. But today is another challenge for us...
While in the OR, many attempts were made to get a central line into Rebekah. This is necessary for two reasons. 1) She has been without nourishment for over 5 days; and 2) The infectious disease doctor wants a central line for her UTI antibiotics. Both of these things cannot be done in a regular IV because Rebekah's veins are small and prone to 'blowing'. Dumping these things into her tissues can cause another set of problems. So we had an appointment with the PICC team to put in a
PICC line. The 'Peripherally Inserted Central Catheter' would go up her arm, across her chest, and down into the vena cava artery that goes into the heart. This procedure is done under anesthesia using special ultrasound equipment, and this would be the second day in a row of anesthetizing Rebekah. The PICC team was also nervous because a central line from the groin area is typically easier to get into place than a PICC line from the arm.
Well, the doctor performing the procedure is Dr. DeVane. He and his team got the PICC line in first try! I was ecstatic and told him, "You are DeMan for DeVeins!" That made him smile. :-) Everyone was thrilled for this victory, and Rebekah did awesome under sedation. They said that trached kids typically need bagged during the procedure, but all she needed was a little blow by oxygen while under and she came out of it like a champ!
 |
| Rebekah - right after the PICC line procedure, still asleep from the anesthesia. |
Saturday 6/4 - First day post-op that Rebekah has finally started 'waking up' and showing us those beautiful eyes and a few fleeting smiles! She started CPT (chest percussion therapy) three times a day, which is pretty standard post-op to help keep the lungs clear. She's in love with Respiratory Therapist, Josh, and he was the recipient of her first genuine sustained smile in over a week! We also finally started her
TPN (Total Parenteral Nutrition) feeds. Regular IV provides the fluids and electrolytes you need to stay hydrated, but it does not provide your body with nutrition, which is the purpose of TPN. TPN puts directly into your blood stream dextrose, amino acids, sodium, potassium, magnesium, calcium, phosphorus, and lipids (fats). Of course, dumping this all directly into your blood stream also has its own set of risks as it taxes your liver and can cause blood clots. So it contains heparin to help with clotting and daily labs are drawn to tweak the TPN 'recipe' and watch for signs of liver toxicity and nutrient imbalances. The goal is to get her off the TPN as soon as possible, but the gut has to start working first. They expect it to be 4-7 days post-op for her system to be working again (inflamation clear and motility to be restored).
Saturday was also a great day for visitors! Rebekah got to see her brothers, her home nurse, and a special friend that is a doctor, but not one of her GHS doctors. :-) This is the first day in a week we've gotten her to interact.
 |
| Rebekah with her Nurse Becky |
 |
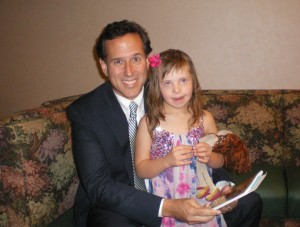
| Rebekah with her special friend, Dr. Putnam |
 |
| Mommy finally getting to hold Rebekah. I had been afraid to hold her since surgery because I didn't want to hurt her tummy. |
 |
| Rebekah's brother, Isaiah, giving her a big kiss. Her brothers miss her a lot! |
Sunday 6/5 - Sunday started with a more fussy baby. Her stomach output doubled from yesterday and I think she is finally starting to feel the pain. Our only options for pain have been tylenol and morphine. Obviously, we don't want to use a lot of morphine since it slows motility and only works for a few hours. We were not allowed to use any motrin products because of her UTI (and possible kidney infection). But thankfully, her urine has been clean for several days, so they finally gave us the OK to use toradol (an effective motrin product that comes in IV form). We can only use this for a short period due to liver toxicity, but it did the trick and seemed to get her over the pain hurdle!
Today we've had our usual bloodwork, and abdominal and chest x-rays. Chest is clear and ab x-rays still show barium just sitting in her system going nowhere. No poop or evidence of bowels 'waking up'. We are pretty much in 'wait' mode...
Monday 6/6 - More waiting... waiting for her bowel to wake up, waiting for her to poop, waiting for her incision to heal... Daily blood work leads to a little tweaking of TPN feeds. We did have a first very small bowel movement, but no real good bowel sounds, so that is the extent of today's excitement. I put a call out to my friends to sit with Rebekah on Wednesday this week so I can spend a day with my parents. They have to leave on Saturday. I was overwhelmed by the response of volunteers! Right now, we are in a good spot, and the calm before the storm...
 |
| Rebekah's tummy must be feeling better because she was pulling her legs up and kicking away! |
 |
| Dear Lord, Thank you for making me feel better. Now please help me to poop today! Amen |
CAMP GHS -
Here is my story to tell for this part of our 'Camp GHS' (Greenville Hospital System) stay -
The one thing that makes me very sad about being in the hospital is the fact that we are missing our one true summer family vacation that we had scheduled a year ago. It is to a place called
Camp New Hope near Boone, NC. It is for children with life-threatening disorders and their families. We went last year and had so much fun! It is a great time of respite because they fully stock your kitchen for you and pretty much take care of everything. We have use of a
Kubota to explore the 160+ acres of mountain trails, there are canoes, tubes and fishing poles for water fun, and all kinds of activities to keep us occupied. We
really needed this respite time as a family.
One of the days Rebekah was still out of it, we had a nurse that was pretty hands off. She pretty much told me the the diapers and general needs were my job. I chatted with her a little bit and was explaining how we had to cancel our vacation to Camp New Hope. She asked me what Rebekah would even do there (that she couldn't do at home, I assumed). And she later asked my husband if she 'does anything'. I feel really sorry that she is a pediatric nurse and she doesn't have the compassion or understanding to take care of special kids without insulting their families. I guarantee that Rebekah can do plenty, and she steals the heart of all who meet her! But even if she DIDN'T, that is not really relevant to the care she should receive.
That coupled with my sadness at missing Camp New Hope had me really bummed. But I really started thinking about the timing of events and realized that God is watching out for us always! Had this all occurred when we were in the middle of the NC mountains, I probably would've tried to treat her longer at 'home' before taking her to an ER. And I am pretty sure there is not a children's hospital anywhere near the camp. So we probably would've ended up at a general hospital with no peds focus. If we managed to get to a children's hospital, it probably would have been out of state and with doctors who don't know anything about Rebekah other than "she has trisomy 18". It really could've been a bad situation, and just the logistics of how we would manage the kids boggles me. But instead, we had a week where grandparents were able to come help us, she stayed local with doctors who already know how amazing she is, and our life wasn't thrown upside down by being out-of-state. Praise God for this stay at Camp GHS! It may not be where I want to be, but I know He has His hands on the situation.